Oxygen Therapy
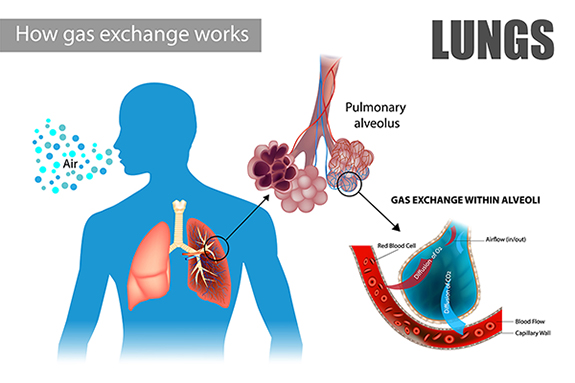
Oxygen is a naturally occurring gas in the air that we breathe. It is essential for life. Normal air contains approximately 21% oxygen. When we take a breath in, the oxygen travels into our airways down to tiny air sacs called alveoli. Alveoli are surrounded by tiny blood vessels called capillaries (kAp-uh-le-reez). As oxygen moves into the capillaries, carbon dioxide (kAHR-buhn die-AHk-sied), a waste gas, moves from the capillaries into the alveoli. After this switch happens, the heart then pumps oxygen around the body and the waste gas is removed as we breathe out. In patients with severe bronchiectasis and NTM lung disease this process can be disrupted due to damage to the lungs from chronic inflammation and mucus pooling. If this happens, a person may need oxygen therapy (also known at supplemental oxygen).
Supplemental oxygen is a medical treatment that is prescribed by your doctor. By adding additional oxygen to the air that you breathe, you can feel less breathless, improve your quality of life, reduce strain on your heart, and prolong your life expectancy by reducing the risk of other complications associated with bronchiectasis and NTM lung disease.1,2
How do I know if I need supplemental oxygen?
It may be hard to know when you need supplemental oxygen. If the oxygen level in your blood is low, you may have symptoms like shortness of breath, fatigue, swelling of your ankles, anxiety related to exertion, and/or headaches.3 If you feel any of these symptoms, talk to your doctor about checking your oxygen levels.
You may also want to think about purchasing a pulse oximeter (ahk-sIm-uh-tuhr) in order to monitor your oxygen levels. A pulse oximeter (also known as pulse ox) is a small personal oxygen meter that you place on the tip of your finger. The pulse ox gives you a measurement of your oxygen level quickly and painlessly. There are several factors that can cause it to read incorrectly (e.g., cold fingertips, movement, poor circulation, dark nail polish); however, it is an easy way you may be able to keep an eye on your oxygen levels at home.

What tests can be done to see if I need oxygen?
A clinician will most likely check your oxygen levels in the office, both while sitting and while doing some basic activities like walking, to see if your oxygen levels are high enough even with activity. During this test, if your oxygen level drops too low (usually less than 88%), you might need oxygen with activity. Another test that can be done is an arterial blood gas (ABG). This test is done by taking a blood sample from an artery (blood vessel that carries oxygenated blood) and analyzed to give your clinician results with more detailed information on how your lungs are working.3 If either of these tests shows you need supplemental oxygen, your clinician will write a prescription for it. The prescription will tell you a “flow rate” and when you should use your oxygen (e.g., continuously or only with activity).
How do I choose a supplier?
Once you have an order for supplemental oxygen, you then must choose an oxygen supplier.
Questions to ask a potential oxygen supplier:
- Are you a national company? Where is the nearest location?
- What systems do you provide?
- What will my out-of-pocket expense be with my oxygen system?
- How often will oxygen be delivered to my home?
- How often will equipment be checked or serviced?
- Will I have an oxygen system that will allow me to travel?
- Who do I call in an emergency? What is your typical response time?
- Do you have any customer feedback that you can share?
- Are you licensed or accredited? By which groups?4
Oxygen systems and devices
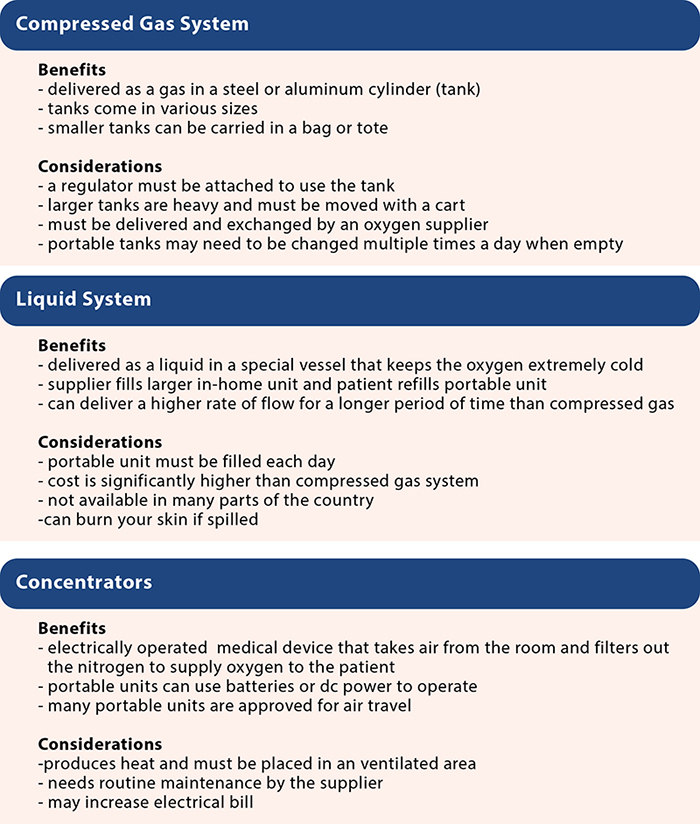
Not all oxygen systems are created equal. There are three types of oxygen systems: compressed gas, liquid, and concentrators. It may be important to learn about the pros and cons of using each system before you decide which one to use. Some oxygen suppliers may give you the option of choosing a system for use in the home and a different system to use when you are away from home.
Oxygen delivery devices – There are several ways in which you can get the supplemental oxygen from the system into your body.
Nasal Cannula (CAN-you-luh) – The nasal cannula is the most common delivery device. A small tube runs from the oxygen source to two small plastic prongs that rest in your nose. The tubing stays in place by looping over your ears. The standard nasal cannula can accommodate 1-6 liters per minute (lpm) of oxygen flow. If you are noticing that your nose and sinuses are drying out, ask your oxygen supplier if you can get a disposable bubble humidifier bottle to provide some humidity.
High Flow Nasal Cannula - These cannulas look very similar to the standard nasal cannula but are slightly wider to accommodate higher flow rates. Often high flow nasal cannulas are heated and used with a humidifier, so it is more comfortable and does not dry out the upper airway.
Oxygen Reservoir Cannula – This type of nasal cannula has a pouch or pendant that can store extra oxygen. When you take a breath in, the stored oxygen will add to your normal flow providing you a larger amount of oxygen as you inhale. Oxygen reservoir cannulas typically must be prescribed by your clinician in order to be given to you by your oxygen supplier.
Other considerations
Safety
Oxygen should never be used around open flames as it will make any fire or spark burn hotter and faster. There are safety measures that you can take to keep you and those around you safe.
- Never smoke or allow anyone to smoke around you while around your oxygen equipment.
- Do not use oil or petroleum products while wearing oxygen.
- Never use oxygen around an open flame.
- Store your oxygen equipment securely and at least 10 feet away from stoves, fireplaces, and other places where sparks can occur.
- Post signs that oxygen is in use.
- Always use the appropriate bag, tote, or cart for transporting oxygen safely.
- As a precaution, tell your local fire department and electricity provider that you use oxygen therapy. They may designate you as a priority during a power outage.
- Be careful around oxygen tubing to avoid tripping.
- Do not try to fix broken equipment yourself.4

Emergency preparedness
- Many home concentrators do not have a battery source for backup power. Ask your oxygen supplier if you can store an extra tank in the event that you lose power.
- Tell your power company that you use oxygen and fill out any necessary forms that will make you a priority during power outages.
- Always have working smoke alarms and a fire extinguisher close by.
- Consider buying a backup generator in the event of a power outage.
- Keep a close eye on your oxygen supply to give your supplier enough time to deliver refills.5
Lifestyle
You may be concerned about how using supplemental oxygen can affect your lifestyle. Many people who first use supplemental oxygen are overwhelmed and self-conscious. Using supplemental oxygen will take some time to get used to.
- Take time to educate yourself on your oxygen system. If you use tanks, practice changing the regulator. If you need to wear it continuously, start by taking short trips out to get used to moving the oxygen device in and out of your vehicle. Allow extra time to get to your destination.
- Adapt your favorite activities. Whether you love to golf, swim, hike, or bowl, find ways in which you can still participate in these activities while still wearing your oxygen. Do not give up your favorite pastimes—find a new way of doing them!
- Do not let wearing supplemental oxygen discourage you from socializing with family and friends. Although your loved ones are not yet used to seeing you wear oxygen, they still want to spend time with you. The more often they see you wearing it, the less unusual it will be.
References
1British Lung Foundation. Home Oxygen Therapy. https://www.blf.org.uk/support-for-you/oxygen/how-does-it-help. Accessed May 11, 2021.
2Chest Foundation. Bronchiectasis Lung Health A-Z. https://foundation.chestnet.org/lung-health-a-z/bronchiectasis/?Item=Treatment. Accessed May 11, 2021.
3National Jewish Health. On the go with oxygen. https://www.nationaljewish.org/conditions/medications/on-the-go-with-oxygen. Accessed May 11, 2021.
4COPD Foundation. Oxygen Therapy. https://www.copdfoundation.org/Learn-More/I-am-a-Person-with-COPD/Oxygen-Therapy.aspx. Accessed March 12, 2021.
5American Lung Association. Using oxygen safely. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/oxygen-therapy/using-oxygen-safely. Accessed May 24, 2021.