Bronchiectasis Frequently Asked Questions (FAQs)
What is bronchiectasis?
It is a lung disease with enlarged airways that are thickened and/or scarred. This can cause mucus to build up in the lungs. Excessive mucus build-up in the airways may lead to repeated infections causing more lung damage.
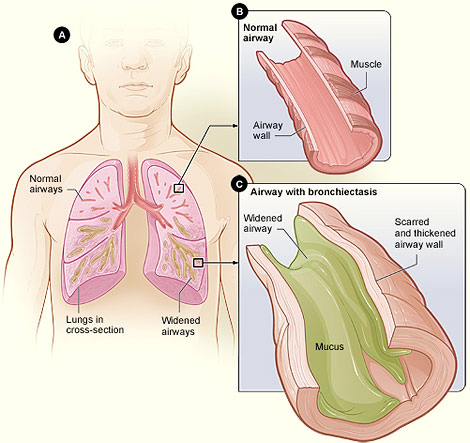
Figure A shows a cross-section of the lungs with normal airways and with widened airways. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway with bronchiectasis and mucus. Illustration courtesy of National Heart, Lung, and Blood Institute; National Institutes of Health; US Department of Health and Human Services.
Normal lungs have built-in systems to stay clean and clear of mucus. Mucus from the lungs is called sputum or phlegm. In healthy lungs, cilia (tiny hair-like structures) move normal amounts of mucus out of small airways into large airways and then the throat. With bronchiectasis, cilia do not move as well, and mucus is more likely to build up in the airways. Failure to clear mucus can lead to bacterial growth, repeated infections, airway damage and more severe disease with worsening airway enlargement.
What are the symptoms?
- Frequent coughing (often with thick, discolored mucus in varying amounts)
- Sputum production
- Breathlessness
- Repeat chest infections
- Increased tiredness
- Unexplained fever, chills, sweats and weight loss
- Chest pain
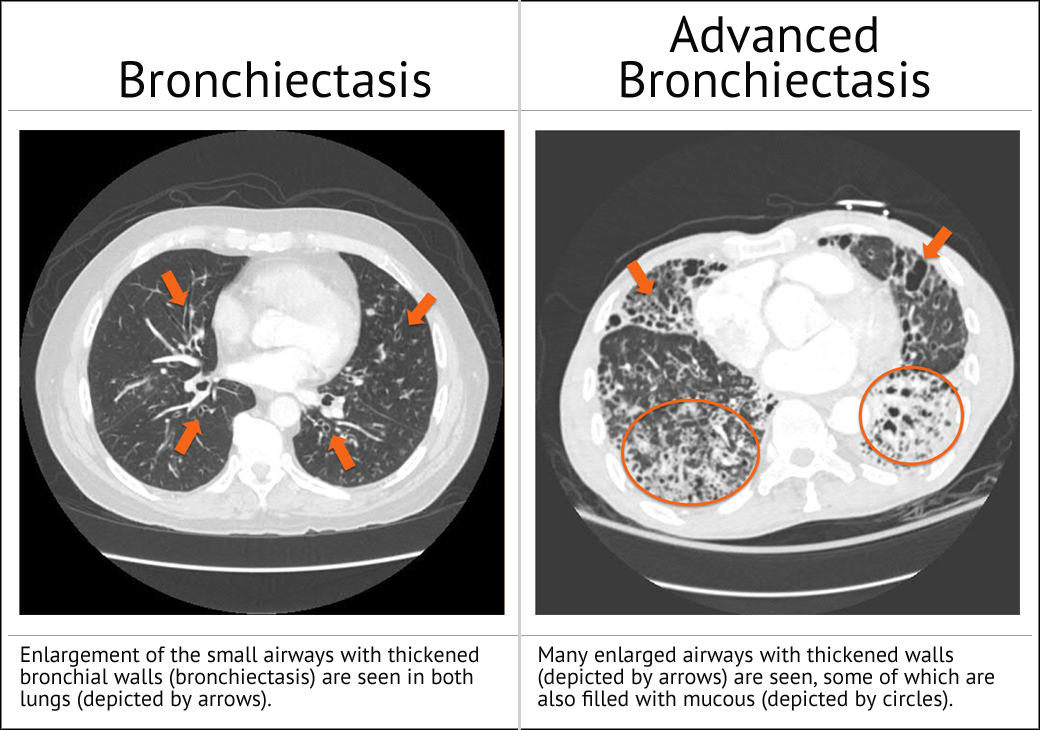
How is bronchiectasis diagnosed?
Bronchiectasis is typically diagnosed by high resolution computed tomography (HRCT) scan – a form of x-ray that gives a very detailed picture of your lungs. The image will show the location of the disease within the lung, as well as the extent of lung damage.
What other medical tests/procedures are common for bronchiectasis patients?
Other tests that bronchiectasis patients may be asked to complete include:
- Pulmonary function tests (PFT) – breathing tests that are administered by trained health care workers to measure how well your lungs are working.
- Sputum sample – a sample of mucus from your lungs is collected and analyzed to see if any abnormal bacteria or fungi grow in the sample.
- Blood sample – occasionally, blood tests are used to help identify medical problems that can either cause or increase the risk of bronchiectasis
Is it contagious?
No, the disease is not passed from person to person. It is also unlikely for others to get sick from you but, people with bronchiectasis are more likely to get sick from others. Washing hands regularly to avoid illness is encouraged.
What are the causes?
About half of the time, the cause is unknown. This is called “idiopathic.” The causes of bronchiectasis include:
- Idiopathic bronchiectasis where a cause is not found, even after testing.
- Other causes include infectious, inflammatory, or allergic diseases. A severe infection, such as a pneumonia, can damage the lung and lead to bronchiectasis. An example of an allergic disease is allergic bronchopulmonary aspergillosis (ABPA). Aspergillus is a type of fungus and sometimes referred to as a mold. Nontuberculous mycobacterial (NTM) lung infections, inflammatory bowel disease, and frequent aspiration (inhaling food and/or stomach contents into the lungs) are other causes of bronchiectasis.
- Frequent lung infections can be caused by a weakened immune system. Some people are born with a weak immune system, but others can develop a weak immune system later in life.
- Cystic fibrosis (CF) is the most common of all the genetic causes of bronchiectasis. It is often found by newborn screening, but sometimes it is found in teens and adults. Testing for CF requires a sweat chloride test and/or genetic testing.
- Primary ciliary dyskinesia (PCD) is a genetic disorder linked to slowed movement of the cilia in the airways. This causes repeat ear infections, sinus infections and bronchiectasis. PCD is found by testing for nasal oxide levels, looking at cilia under a microscope and/or genetic testing. There is often a history of pneumonia and sinus infections or breathing problems soon after birth.
What are the treatments?
Regardless of the cause, there are two key parts to proper treatment. First, it is important to remove mucus from the airways (maintain airway clearance) and secondly, to treat infections.
It is important to keep sputum moving up and out of the lungs to avoid pooling of mucus and infections. This can be done in several ways:
Treating Infections
It is vital for your health care provider to know what infections are present in order to treat them with the proper medicines. This process involves collecting a sputum sample to find bacteria, fungi (mold) or mycobacteria that are present in the airways. Some health care providers test the sputum as often as every three months, even when the person is not sick. This allows them to monitor what germs may be growing in the mucus that may need to be treated.
What is an exacerbation?
This occurs when bronchiectasis suddenly gets worse and makes a person sick. This is often called a flare-up. Treatment for a flare-up may differ from other lung infections. It may need a longer course of antibiotics or a combination of antibiotics. These may be given by oral, inhaled or intravenous (IV) routes. It is important to tell a health care provider about early warning signs of a flare-up so treatment can be started right away.
Is there a cure?
There is no cure for bronchiectasis, but it can be treated. Watch for early warning signs of a flare-up and work with a health care provider to find the best treatment plan. In a few rare cases, surgery to remove damaged lung tissue, found in only one area of the lung, may be curative. Research and clinical trials are taking place now to find better treatments and cure(s) for bronchiectasis.