Manual Airway Clearance Techniques
Chronic cough is a major symptom of bronchiectasis. This is caused by too much mucus in the lungs and expanded airways that makes it hard to cough out the mucus. Tiny hair-like structures in the lungs, called cilia, move mucus out of the small airways. In bronchiectasis, the cilia are often damaged because of a thickening of the airway wall. This also makes it difficult to cough out mucus. As an individual with bronchiectasis, it is important that you use good techniques to clear your lungs. This can include directed coughing and/or postural drainage (see below). Mucus left in the lungs can lead to an infection, inflammation, low oxygen levels, and/or a collapsing of the airways (also known as atelectasis).1 Repeated infections can lead to your bronchiectasis becoming worse.
Directed Cough Techniques
You may wonder why you should make yourself cough. The reason is to keep mucus from pooling in your lungs. Mucus pooling can allow bacteria to enter the lungs which can cause an infection. Directed cough methods use deliberate coughing to clear mucus from the airways. Below are a few different types of directed coughing methods often used by individuals with bronchiectasis. Often, directed cough methods are used with inhaled medicines and with postural drainage therapy.
Deep Cough
Begin by sitting upright and taking a couple of normal breaths through your nose and out through pursed lips. Next, take a deep breath in and hold it for 2-3 seconds. Then use your stomach muscles to help force the air out of your lungs in a deep cough. This should move the mucus out of your lungs allowing you to cough it out.2 Remember to take several normal breaths before trying another deep cough.

Huff Coughing (forced expiratory technique or FET)
Huff coughing, or huffing, helps move mucus from the lower airways to the upper airways. This happens through a series of quick, forced breathing out or “expiratory” exercises.2 Start out by taking a few deep breaths. Next, take a large breath in and use your stomach muscles to breathe out in three short, rapid breaths while making a “ha, ha, ha” sound. This sound should come from deep down. Squeeze your stomach muscles in. Follow-up with some deep breathing and perhaps a deep cough to help clear any mucus that you may have moved or “shaken loose." Remember to pause and rest after each huff cough and before you try again.
Splinting
Sometimes, you may experience pain or soreness in your ribs or chest wall when coughing. Splinting is a method used for people who have had recent chest surgery, have broken ribs, or feel their chest wall is “unstable.” By using this method, you may get a better cough. Grab a pillow or a large stuffed animal. Hold it up to your chest. As you cough, squeeze it with your arms close to your chest. *Notify your physician if your rib pain persists.
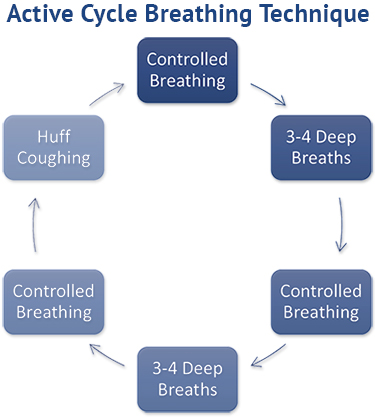
Active Cycle Breathing Technique (ACBT)
Active cycle breathing techniques combine controlled normal breathing, deep breathing using the stomach muscles, large breath holds, and huff coughs.3
To perform an active cycle breathing technique, follow these steps3 in order:
- Perform controlled breathing by focusing on breathing in and out steadily for 20-30 seconds; relax your chest and shoulder muscles.
- Take a large breath in using your stomach muscles to draw the air into the lungs. Hold the breath for 3 seconds. Do this 3-4 times.
- Do controlled breathing again—focusing on breathing in and out—for 20-30 seconds.
- Take a large breath in using the stomach muscles to draw the air into the lungs. Hold the breath for 3 seconds. Do this 3-4 times.
- Do controlled breathing again—focusing on breathing in out steadily—for 20-30 seconds.
- Do huff coughing (see above).
Postural (Autogenic) Drainage and Chest Physical Therapy (CPT)
Postural (Autogenic) Drainage
An important goal for those with bronchiectasis is to prevent mucus from pooling in the lungs. Postural drainage (often referred to as autogenic drainage) uses gravity, deep breathing, and breath holds to drain the mucus from specific areas of the lung into the larger airways so that it can be coughed out.4,5 Postural drainage is best done after medicine has been inhaled and before meals. To perform postural drainage, lie or sit with the infected lung up. Stay in that position for 10-15 minutes while you take deep breaths, sometimes using a 2-3 second breath hold. Pillows, soft cushions, or bundled blankets may be used to position your body. This may help your lung to drain better.6 Once you have drained each portion of your lung for 10-15 minutes, or if you start to notice more congestion, use a directed cough method to cough the mucus out of your lung. *Ask your doctor to show you which position may help you the most.
Chest Physical Therapy (CPT)
Manual chest physical therapy uses postural drainage, percussion (beating on the back), and vibration of the chest to move mucus to the large airways. CPT sessions are usually done after medicine is inhaled. These sessions usually last 20-30 minutes and can be physically difficult for the care provider. This method is not often used often in the home setting but, it is an effective way to remove mucus from the lungs.7
References:
1Gosselink R. Physiotherapy in respiratory disease. Breathe. 2006 Sep;3(1):30-39
2Fink JB. Forced expiratory technique, directed cough, and autogenic drainage. Respir Care. 2007 ;52(9):1210-1221; discussion 1221-1223.
3Elsayed, Shereen & Abdelbasset, Walid & Fathy, Karim. (2015). Impact of active cycle of breathing technique on functional capacity in patient with bronchiectasis. Int J Ther Rehabil Res. 2015; 4:287-293. doi: https://doi.org/10.5455/ijtrr.000000105
4Cystic Fibrosis Foundation. An introduction to postural drainage and percussion. Cystic Fibrosis Foundation website. Updated 2012. Accessed March 2021. www.cff.org/PDF-Archive/Introduction-to-Postural-Drainage-and-Pecussion.
5Poncin W, Reychler G, Leeuwerck N, et al. Short-term effect of autogenic drainage on ventilation inhomogeneity in adult subjects with stable non-cystic fibrosis bronchiectasis. Respir Care. 2017;62(5):524-531. doi: https://doi.org/10.4187/respcare.05194
6Fink JB. Positioning versus postural drainage. Respir Care. 2002 Jul;47(7):769-777.
7Egan AM, Clain JM, Escalante P. Non-antimicrobial airway management of non-cystic fibrosis bronchiectasis. J Clin Tuberc Other Mycobact Dis. 2017; 10:24-28. doi: https://doi.org/10.1016/j.jctube.2017.12.003