Exacerbations
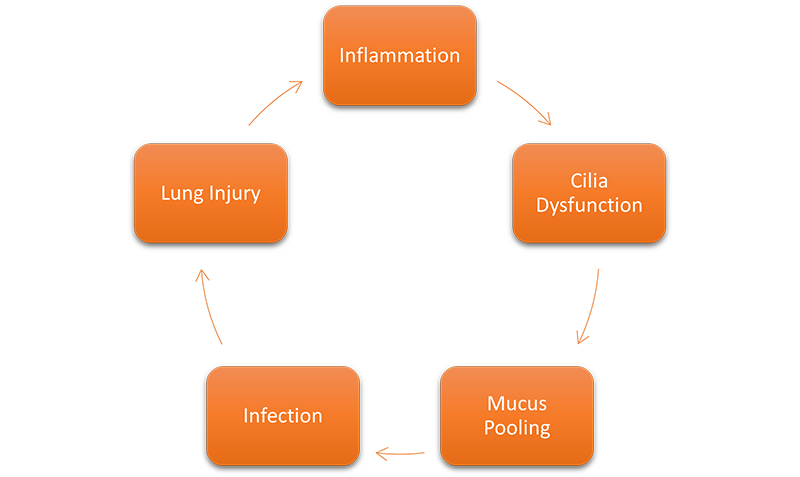
People with bronchiectasis and NTM lung disease sometimes struggle with staying well. Inflammation coupled with mucus pooling in the lungs becomes a breeding ground for bacteria. If you are unable to clear the mucus from your airway, you may have a greater chance of having an exacerbation (x-saa-cer-bay-shun) of your disease. An exacerbation is a sudden worsening of symptoms that may require medical attention. It is frequently referred to as a “flare” or a “flare-up.” How often you have an exacerbation can strongly affect your quality of life and how quickly or slowly your disease progresses.1 As noted in the figure below, bronchiectasis patients who have flare-ups often become trapped in what is called “Cole’s vicious cycle.”1
Early Warning Signs of an Exacerbation and “Red flags”
If 3 or more of the following areas become worse for you within 48 hours, you are having an exacerbation:
- Cough
- Changes in the amount of mucus coughed up and/or texture
- Coughed up mucus is yellow/green
- Feelings of shortness of breath and/or ability to handle exercise
- Feeling tired
- Coughing up blood
AND a change in treatment is decided by a doctor.2
If you are having these warning signs, contact your doctor right away. Delaying treatment may make it harder for you to recover. Your condition could become worse.
Other “red flags” or signs that you need to call your doctor are:
- Fever
- Unusually low oxygen levels (based on your pulse oximeter reading)
- Increased use of “rescue” or fast-acting breathing medicines
- Chest pain
- Blue color in lips or fingers3
How are Exacerbations Treated?
Most exacerbations are caused by a bacterial infection. These infections are treated with antibiotics.1 There are many different types of bacteria. To understand which type is causing your infection, a sample of your coughed up mucus, or sputum, will be collected. The sample will help your doctor know which medicine(s) to prescribe for you to treat the infection.1 Your doctor may also make changes to your regular medicines to target specific bacteria found in your sample. A chest x-ray or CT scan of your lungs may also be ordered, to check for pneumonia. The antibiotics (anty by ahh ticks) prescribed by your doctor may be taken for a short or long period of time.4 If your symptoms get worse or you need to have the antibiotics put directly into your blood intravenously (in traa vee nus lee), you may have to be admitted to the hospital.

How to Reduce Your Chance of an Exacerbation
You cannot prevent all exacerbations from happening. You can work to reduce how often you have them. You can do this by practicing good airway clearance techniques. If you find that your current airway clearance technique is not working well, talk to your doctor about other techniques and/or devices that may help.
Other tips for preventing exacerbations or flare-ups include:
- Practicing good handwashing;
- Distancing yourself from people who have coughs or colds;
- Wearing a mask when in or around large crowds;
- Getting the flu vaccine each year (talk to your doctor to see if he/she recommends getting the pneumonia vaccine also);
- Taking all medicines as prescribed by your doctor;
- Seeing your doctor as soon as you start becoming ill (this may require you to seek urgent or emergency care if it is outside normal business hours);
- Getting plenty of rest;
- Eating well;
- Quitting smoking5
Make a Plan
Talk to your doctor about the best way to contact him/her when you are experiencing an exacerbation. Your doctor may have other instructions or changes for you to make with your treatments or airway clearance routine. Create an emergency action plan for your loved one or caregiver. Consider creating an advance directive so that in an emergency, your loved ones are aware of your wishes regarding your care.
References:
- Polverino E, Rosales-Mayor E, Torres A. Exacerbation of bronchiectasis. In: Chalmers J, Polverino E, Aliberti S. (eds) Bronchiectasis. Springer;2017:205-222. doi: https://doi.org/10.1007/978-3-319-61452-6_15
- Hill AT, Haworth CS, Aliberti S, et al; EMBARC/BRR Definitions Working Group. Pulmonary exacerbation in adults with bronchiectasis: a consensus definition for clinical research. Eur Respir J. 2017 ;49(6):1700051. doi: https://doi.org/10.1183/13993003.00051-2017
- COPD Foundation. What is an exacerbation or flare-up? COPD Foundation website. Updated May 17, 2021. Accessed April 19, 2021. https://www.copdfoundation.org/Learn-More/I-am-a-Person-with-COPD/What-is-an-Exacerbation.aspx.
- National Jewish Health. Bronchiectasis treatment. National Jewish Health website. Published December 1, 2017. Accessed April 19, 2021. https://www.nationaljewish.org/conditions/bronchiectasis/bronchiectasis-overview/treatment.
- American Lung Association (ALA). Treating and managing bronchiectasis. ALA website. Published March 26, 2020. Accessed April 19, 2021. https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/treating-and-managing.